Home
Water Solutions
SOURCE WATER QUALITY
SOURCE WATER QUALITYThe effectiveness of microbial treatment products
Municipal water quality is highly variable depending on your location. This chemical variability can undermine the effectiveness of microbial treatment products like straws and tablets and potentially reduce the life of your instruments.

DENTAL UNIT WATERLINE MANAGEMENT
DENTAL UNIT WATERLINE MANAGEMENTRisk of waterborne infections
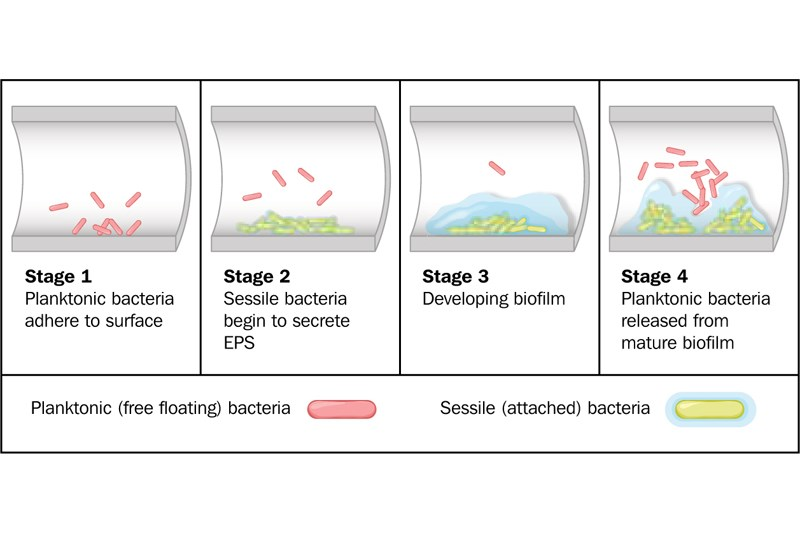
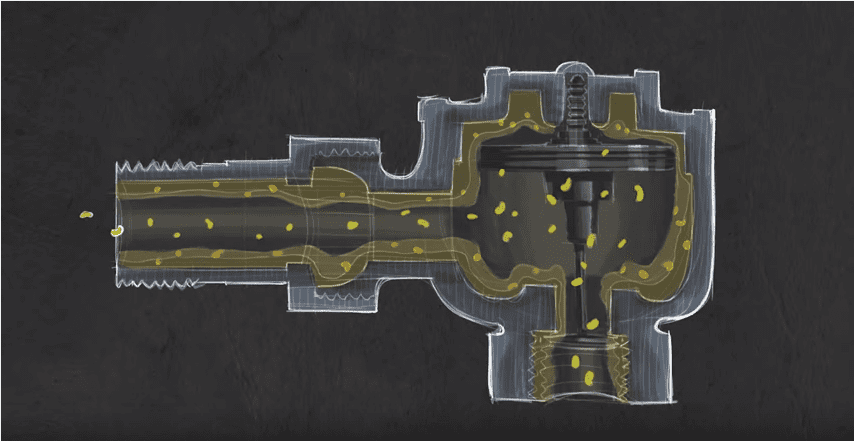
Dental unit waterline (DUWL) management is vital in dentistry to control biofilm buildup, minimize the risk of waterborne infections, and maintain the quality of the dental water supply to ensure safe and effective dental treatment for patients.

ISOLATION AND AEROSOL CONTROL
ISOLATION AND AEROSOL CONTROLProtect the health and safety of patients and dental staff.
Isolation and aerosol control are essential in dentistry to prevent the spread of infectious diseases, reduce the risk of cross-contamination, and protect the health and safety of patients and dental staff. These measures can help minimize the production and dispersion of aerosols during dental procedures, reducing the risk of transmission of airborne pathogens.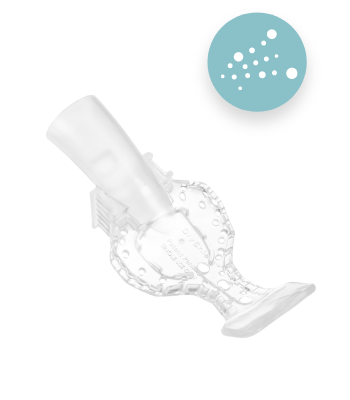
EVACUATION
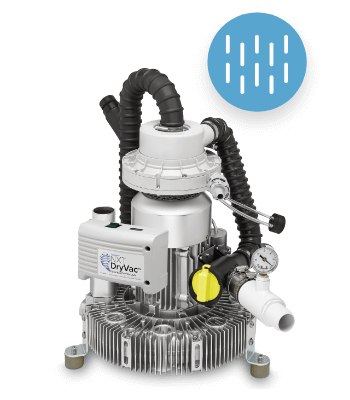
EVACUATIONOur evacuation product solutions include NXT® DryVac, DryShield®, and PowerScrub™
NXT DryVac is a tankless dry vacuum system that provides superior performance with low acquisition costs and virtually no maintenance, all in a compact footprint for easy installation.
AMALGAM CAPTURE AND RECYCLING
AMALGAM CAPTURE AND RECYCLINGAccommodates up to 10 operatories
Featuring top-tier technology, the NXT Hg5 represents the gold standard in amalgam separation for your office. Our signature separator—the NXT Hg5—comes in several sizes to fit the needs of your practice.

WASTE MANAGEMENT
WASTE MANAGEMENTOur Waste Management product solutions includes the PWS
Waste management is essential in dentistry to reduce the environmental impact of dental practices, prevent the spread of infectious diseases, and comply with regulatory requirements.

Products
- SOLMETEXSOLMETEX PRODUCT SERIES
Take advantage of limited time offers on key Water Solutions today!
Solmetex provides dental practices with simple, safe, and effective solutions for removing harmful contaminants from their water supply, enabling safe disposal and recycling of hazardous waste, and best-in-class products for wastewater evacuation.

- STERISILSTERISIL
Sterisil® Water System
Sterisil ensures water for non-surgical procedures is clean and safe by offering effective, and convenient water purification, treatment, and testing solutions.

- DRYSHIELDDRYSHIELD
DryShield® Autoclavable All-In-One Isolation System
DryShield leads the market in providing clinicians with isolation technology that maximizes ease, comfort, safety, and productivity.

- SOLMETEX
Resources
- EDUCATIONEducation
Dental Water Safety Education
Expand your dental water safety knowledge with resources like CE courses, tutorials and videos, and the Water Matters blog.
- CUSTOMER RESOURCESCUSTOMER RESOURCES
For over 25 years, Solmetex has been an innovator in dental water safety.
Today, dentists count on us to deliver a reliable system of solutions to manage the water in, through, and out of the their practice while enabling compliance within an ever-changing regulatory environment.

- DEALER PORTAL
DEALER PORTAL
Your resource for dealer and technical product information
Solmetex recognizes that without the loyal support of our dental suppliers, much of our success would not be possible.

- DOCUMENT LIBRARYDocument Library
Find documents and resources for our products
Download instructions for use, installation manuals, sell sheets, and log sheets.

- COMPLIANCE INFORMATIONWater Safety Compliance Information
Stay up-to-date on EPA dental regulations.
Download a compliance checklist, access state compliance reports, and browse water safety compliance materials.
Request a Sterisil SMART Compliance binder here.

- TECHNICAL TRAININGTechnical Training
Download related technical documents for Solmetex®, Sterisil®, and DryShield® products.

- ARMY CERTIFICATIONSArmy Certifications
Download your training and certification testing resources here.
Password required.

- EDUCATION
Promotions
- PromotionsPROMOTIONS
All deals available now!
Find our current promotions for Solmetex, Sterisil and DryShield in one place.

- Promotion SubmissionPROMOTION SUBMISSION
Process your rebate and/or your free product.
Find our current promotions for Solmetex, Sterisil and DryShield in one place.

- DryShield Free TrialDRYSHIELD FREE TRIAL
Try the DryShield isolation system free for 30 days!
The DryShield Free Trial Kit includes the DryShield Isolation System along with an assorted sample pack of both our Autoclavable and Single-Use Mouthpieces.

- Endorsements/PartnershipsEndorsements
Find our endorsed products by State, local Dental Associations and Societies.
These special partnerships enable members to receive special programs and services as a membership benefit.

- Promotions
My Solutions Center
- Compliance CenterCOMPLIANCE CENTER
Follow Regulations
Make sure your office stays compliant with EPA and state regulations.
- RECYCLING CERTIFICATESRECYCLING CERTIFICATES
Access Documents
Keep track of your amalgam waste recycling certificates.

- WATER TESTINGWATER TESTING
Track Results
Log, trend, and respond to ongoing bacteria testing efforts.

- SUBSCRIPTIONSSUBSCRIPTIONS
Set Up Deliveries
Schedule your orders to ensure you are never without products.

- PRODUCT REGISTRATIONPRODUCT REGISTRATION
Enroll Products
Register your water safety products and receive proof of installation certificates.

- CREATE SUPPORT CASECREATE SUPPORT CASE
Report Issues
Request customer support and track your case to its resolution.

- Compliance Center
Support
- SUPPORTSUPPORT
Expert Support
We have extensive experience in
water chemistry, chemical separation science, process engineering,
high performance manufacturing, as well as federal, state and local
regulations governing water and hazardous wastes.
- SPECIAL MARKETSSpecial Markets
Unlock enterprise-level results by leveraging our expertise across clinical and corporate domains to implement tailored practice-level solutions.
Solmetex is proud to partner with over 200+ DSO's, GPO's, Military, and Schools.

- INTERNATIONALINTERNATIONAL
Locate authorized distributors in your region.
Our international dealer directory lists trusted partners selling Solmetex products and solutions in key countries around the world.

- WATER CONSULTATIONWater Consultation
Schedule a free water consultation with a Solmetex Water Solutions Expert.

- SUPPORT
RECYCLE, SHIP, ORDER NOW
RECYCLE, SHIP, ORDER NOW
- Print Recycle Shipping LabelShipping Labels Made Easy
Print Recycle Shipping Label
Print and place your shipping label on the box containing your recyclables.
- Print Recycle CertificateRecycling Made Easy
Print Recycle Certificate
Print and place your recycling certificate on your full amalgam separator canister, or lead buckets to be EPA-compliant.
- Order NowProduct Ordering
End-to-End Dental Water Management Products
Purchase products for all your dental water management needs from Solmetex, Sterisil, and DryShield.
- Print Recycle Shipping Label
Municipal Tap Water
Ultraviolet Dental Waterline Disinfectants – A Dental Healthcare Providers Guide
July 4, 2023
Dental Waterline Testing – A Crash Course in Commonly Accepted Methods
July 6, 2023Municipal Tap Water
Hey you, yeah you, filling that dental bottle at the faucet. How clean do you think that water is? Have you checked to see if there were any boil water alerts lately? Do you have any filtration or purification in place for that supply? Are you assuming that water is clean enough for use in the dental chair, or do you know for sure? I hope you have some sound disinfection protocols in place. If you knew what could be in that water, you might think twice.
When you look deeper into past issues related to pathogens and tap water, the revelations might have you thinking twice about filling that dental bottle at the tap. Independent bottle reservoirs were intended to give practitioners the flexibility to avoid tap water and the potential problems it presents. So why not take advantage of it? Why fill with water from the tap? Doing so would imply that you are either testing routinely or just assuming it is of good quality.
With so much waterline infection control information available, most clinicians know the hard facts that municipal tap water could be contributing to their bacteria problems. Public water works delivering your municipal tap water are prone to contamination and breaches in their own water quality standards. Common events such as a water main break, leak, or drop in pressure, present an opportunity for pathogens to gain access to the public works.
By the Numbers
As of 1971, the Centers for Disease Control and Prevention (CDC), U.S. Environmental Protection Agency (EPA), and the Council of State and Territorial Epidemiologists (CSTE) have been tracking and quantifying these waterborne disease outbreaks in the US. The most interesting insight from the data they provide is that over the 36 year period from 1971 to 2007, “a trend analysis found a statistically significant decrease in the annual proportion of reported deficiencies that were associated with the inadequate or interrupted treatment of water by public water systems[3].
Premises Plumbing
“Health care settings, such as hospitals and nursing homes, were the second most common outbreak location in community systems, highlighting the need for continued vigilance to ensure provision of safe water to locations that serve populations that are more vulnerable, such as hospitalized patients or nursing home residents with preexisting medical conditions[3].”
- American Society for Microbiology
For dental professionals in large healthcare facilities, It is certainly worth considering speaking with building managers about the plans for water treatment within the building. Systems of water quality monitoring and intermittent testing should be in place where the consequences could be serious.

Case in Point

Less is More
Variations in tap water quality are virtually infinite and therefore, tap water should not be relied upon for consistent disinfection results. The presence of municipal additives such as chlorine and fluoride complicates things further if you are trying to manage the chemistry to get the best results. If you don’t, you have a concoction of different chemicals and additives mixing in the waterline. The byproduct of these unwanted mixtures is called “precipitates,” and their presence indicates the diminished effectiveness of whatever you have in the water to control microbes. So what is the solution?

Max Out Your Safety Margin
To attain maximum chemical control, “distilled quality” water works best. We say distilled quality because water from a distiller is not always optimal for dental water. The nature of distillation requires that you heat the water to remove impurities. This hot distillate is now primed for recolonization by bacteria. Without immediate waterline treatment, this water will most assuredly be contaminated by the time it reaches the dental bottle. Distillers themselves are often the source of contamination for many offices as once the storage tank is contaminated, the water is then distributed along with the bacteria to the entire office.
The best strategy is a point-of-use purification system using deionization to remove all the impurities without heating the water. Ultraviolet disinfection can then be employed to drastically lower the existing bacterial load with proven effectiveness[5]. The water would then receive a low concentration of a residual disinfectant. The final product is water that is neutral in pH, contains less than 10ppm total dissolved solids, disinfected, and contains some variety of residual disinfectant.

No Excuses
Attaining and utilizing distilled quality water is easier and more affordable than ever. It’s use protects the dental practice from potential contamination within the public treatment works of which there are numerous cases which have tap water as a contributing factor. Steer clear of distillers, they are often contaminated and are more work to maintain than their deionization counterparts. Distilled water is an essential building block of a successful disinfection protocol.
References
1. Ingerson-Mahar, M.; Reid, A. Microbes in Pipes: The Microbiology of the Water Distribution System A Report on an American Academy of Microbiology Colloquium; ASM Academy: Boulder, CO, USA, 2012; p. 26.
2. RamÃrez-Castillo, Flor, et al. “Waterborne Pathogens: Detection Methods and Challenges.” Pathogens, vol. 4, no. 2, 2015, pp. 307–334., doi:10.3390/pathogens4020307.
3. Craun, Gunther F., et al. “Welcome to CAB Direct.” CLINICAL MICROBIOLOGY REVIEWS, vol. 23, no. 3, July 2010, pp. 507–528., www.cabdirect.org/cabdirect/abstract/20103246391.
4. Peralta, Gianna, et al. “Morbidity and Mortality Weekly Report (MMWR).” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 25 Aug. 2017, www.cdc.gov/mmwr/volumes/65/wr/mm6513a5.htm.OSAP - Dental Unit Waterlines
5. UV Dose Required to Achieve Incremental Log Inactivation of Bacteria, Protozoa and Viruses Gabriel Chevrefils, B.Ing,2 and Eric Caron, B.Sc.2